Recent Innovations and Advancements in Healthcare at Your Fingertips
Penned by medical and scientific experts, writers, and editors
Unbiased data from medical journals, peer-reviewed studies, and research institutions

Meticulous fact-checking for medical, scientific, and analytical accuracy
Leading the way to a healthy community
Meet Dr. Edward Zelman:
The Man Behind PainPathways
Dr. Edward Zelman started PainPathways to help people with chronic pain live a healthier life. The blog provides accurate information on pain management and empowers individuals to define their own path to wellness. It fosters community and collaboration among its readers and partners, making it a valuable resource for anyone seeking support and guidance.

Latest Articles
You may also read
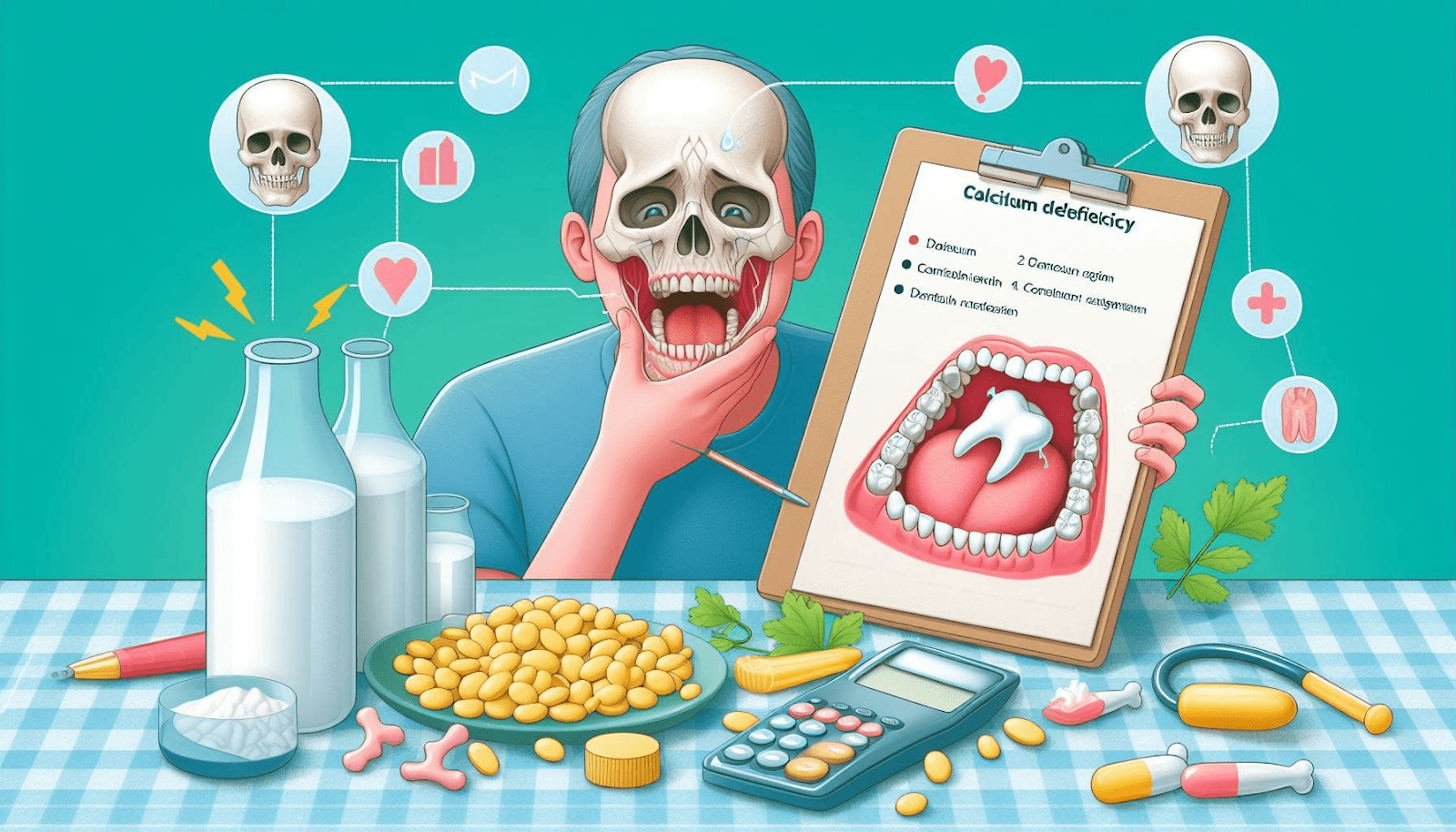
The Consequences of Calcium Deficiency on Dental Health
Calcium is an essential mineral that plays a vital role in the overall health and development of our teeth and bones. Adequate calcium intake is crucial, particularly during childhood and adolescence when the teeth and jaws are still forming. However,…
Normocytic Anemia: Understanding the ICD-10 Coding
Anemia is a common medical condition characterized by a reduced number or volume of red blood cells (RBCs) or hemoglobin in the blood. There are various types of anemia, each…
Is Angioplasty the Most Typical Treatment for Arteriosclerosis?
Arteriosclerosis is a serious vascular condition characterized by the buildup of plaque inside the arteries. This plaque narrows and hardens the arteries, restricting blood flow and oxygen supply throughout the…
Is Jaundice Contagious?
Jaundice is a condition characterized by the yellowing of the skin, whites of the eyes, and mucous membranes. This discoloration is caused by the buildup of a yellow-orange pigment called…
Navigating Complete Heart Block: Understanding the ICD-10 Classification and Comprehensive Management
Complete heart block, also known as third-degree atrioventricular (AV) block, is a serious cardiac condition characterized by the complete disruption of electrical impulses between the atria and ventricles. This condition…