Pediatric Pain Management
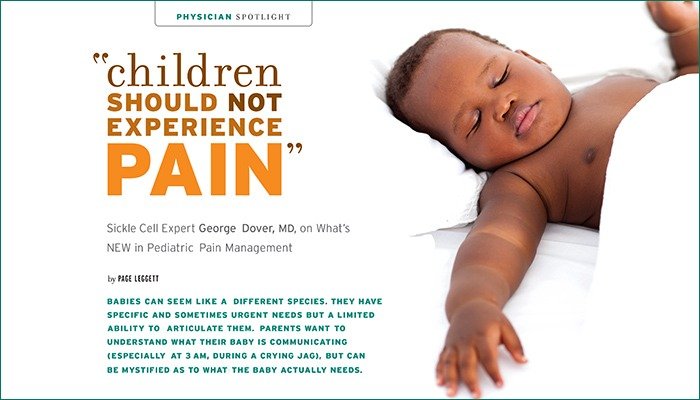
Babies can seem like a different species. They have specific and sometimes urgent needs but a limited ability to articulate them. Parents want to understand what their baby is communicating (especially at 3am during a crying jag), but can be mystified as to what the baby actually needs.
But what babies feel is much more evident to doctors now than it was 40 years ago. “Unbelievably, in the1970s, it was unclear to us if babies could feel pain,” says George J. Dover, MD, professor and director of the department of pediatrics at Johns Hopkins University School of Medicine and pediatrician-in-chief of the Johns Hopkins Children’s Center.
“That thought was based on no scientific data at all,” Dr. Dover marvels.
Parents can thank Johns Hopkins for leading the way in determining that babies experience pain. Johns Hopkins Children’s Center has had a pediatric pain service since 1991and a tradition of pioneering research in pediatric pain management that goes back generations. Dr. Dover gives credit specifically to Hopkins’ own Myron Yaster, MD, a pediatric anesthesiologist and pioneer in child pain research.
Adults may remember seeing a doctor who said “This will only hurt a little” before performing a procedure that may have hurt a lot. Incredibly, that was once the standard of care. Some trained experts would even hold a child down while a doctor performed whatever procedure “hurt a little.” Pediatrics has come a long way since those primitive days.
“We no longer assume anything,” Dr. Dover says. “Now, we ask: ‘Are you in pain? What level?’ Hospitals are measured today by how consistently they monitor patients’ pain levels—and how they address the pain.”
THE SEA CHANGE: PARENT EXPERTS
The sea change, as Dr. Dover calls it, began when doctors started to collaborate with parents whose children were hospitalized. Physicians began to recognize that parents were experts on their children and, in fact, needed to be included in their care plans.
Today, Dr. Dover says the medical community’s philosophy on children and pain is based on this belief: “Children shouldn’t have to experience pain. It’s not an option.”
FAMILY-CENTERED CARE
For more than a century, Johns Hopkins has been a leader in pediatric medicine and research. In 2012, it opened the Charlotte R. Bloomberg Children’s Center (named after New York Mayor Michael Bloomberg’s mother), a 12-story, 205-bed facility where the comforts of home meet state-of-the-art medicine.
Everything about the space is designed to make children and their families feel at ease. It’s a bright, vibrant place where 300 works of art, created by more than 70 artists, animate the hallways.
Ask Dr. Dover why the center is special, and he tells you, “There’s not enough time to list all the reasons, but I’ll say it’s designed to facilitate ‘family-centered care,’ which is different from ‘patient-centered care.’
“The patient’s family is an important part of the team,” he says. “We now have private rooms that include sleeping accommodations for parents inside the room. We did away with specified visiting hours. The doctors don’t make rounds in the hallway anymore; we are at each patient’s bedside. We did away with set times that children have to eat. Even the structure of this place focuses on the needs of the family and the child. There’s been an entire attitude change.”
It’s not that the staff didn’t want to offer family-centered care before. But, Dr. Dover says, the architecture in the old building didn’t allow for it. In the old facility, there’d be two or three pediatric patients to a room—with a curtain separating them—and no room for Mom or Dad to spend the night.
All rooms are now large enough to accommodate family and designed to ensure that no matter the level of care, one room can be used throughout their stay.
It’s not just a new building. “It’s a whole new way of thinking,” says Dr. Dover. “This center is one of the jewels in the crown of Hopkins.”
SICKLE CELL PIONEER
As a pediatrician Dr. Dover manages many childhood maladies, but his specialty is sickle cell disease (SCD), a genetic condition that affects nearly 100,000 Americans—most of them African American, as well as people of Middle Eastern and Mediterranean descent. Named for the distorted, sickle-shaped red blood cells caused by the disease, the condition causes these oxygen-transporting cells to become rigid and sticky, which in turn reduces the amount of oxygen getting to vital organs. This causes severe pain and “sickling crises.” Often, these episodes require blood transfusions and hospitalization.
Dr. Dover didn’t know what SCD was until he began training at Hopkins in 1977. He learned that pain associated with sickle cell disease can present suddenly, and almost anywhere in the body, making it difficult to determine the cause of the pain.
“I remember this so clearly, although it happened years ago,” he recalls. “A teenaged boy—who had sickle cell disease and had been in a car accident that resulted in a compound fracture—came to us. Someone bumped the stretcher he was on, and he winced in pain. I asked him, ‘How did that pain compare with the pain you feel from sickle cell disease?’ He said, ‘This was less severe. And it goes away. That doesn’t happen with sickle cell disease. There’s no way to stop it.’”
So, sickle cell pain was worse and lingered longer than the pain that resulted from a bone sticking out of the skin? Dr. Dover knew he had to study the condition—and work to reduce the pain.
“Pain is a major feature of sickle cell disease,” he says. “If you become a sickle cell doctor, you are committed to treating pain.”
TRUST THE CHILD
Dr. Dover explains that decades ago, there was a common belief—a suspicion, even—that children weren’t in as much as pain as they said they were. Physicians would point to the fact that a child in the hospital was able to fall asleep as “evidence” that his pain wasn’t severe. “We now know you can escape pain by sleeping,” he says. “The fact that a young patient may be asleep doesn’t mean her pain isn’t real. It means her body is physiologically trying to cope with it.
“I was trained at Hopkins,” Dr. Dover says with obvious pride. “Here, if a child says he’s in pain, we treat him as if he’s in pain.”
Dr. Dover’s career is inextricably linked with the place he’s spent its entirety. After earning his medical degree from Louisiana State University Medical School, he trained in pediatrics at Hopkins, where he completed a fellowship in pediatric hematology/oncology before joining the faculty in 1977.
Dr. Dover is gratified to have spent his career at Hopkins. “I’ve got the best job in pediatrics in the country,” he says. “It’s a joy to witness all the innovations by my colleagues that have made such a difference in people’s lives.”
Outside the hospital, Dr. Dover enjoys time with his wife and their seven grandsons, all of whom live nearby.
“My life in the hospital is hectic, and my life out of the hospital is hectic,” he says. “And they both contain children. I’m very lucky.”
ORIGINS of PEDIATRIC PAIN MANAGEMENT
Like Dr. Dover, Sabine Kost-Byerly, MD, the first president of the Society for Pediatric Pain Medicine and Johns Hopkins’ director of pediatric pain management, recalls a time when doctors weren’t sure if babies felt pain. “We thought they didn’t have pain—or, if they had it, that they couldn’t remember it,” she says.
Dr. Kost-Byerly did her pediatric residency nearly 30 years ago. She followed that with a residency in anesthesiology and started a journey that would lead her to become one of the nation’s foremost authorities on managing pediatric pain.
Dr. Kost-Byerly says the groundbreaking research of Canada’s Anna Taddio, BScPhm, MSc, PhD, in the 1990s led doctors to understand that children do, on some level, remember pain. “Anna Taddio found that boys who had been circumcised cried more when they were immunized two or three months later than boys who had not been circumcised. We now understand that the brain remembers pain.”
After doctors came to understand that pain in infants is real, the next step was to find pain management therapies that were safe for tiny bodies. “We didn’t always have good, safe tools to treat newborns and infants,” Dr. Kost-Byerly says. “There was a time when doctors told parents, ‘Your child is too high a risk for anesthesia.’ You don’t hear that anymore.
“There was a lot of compassion-building in the 1980sas parents began to demand better pain management for their children,” she says. Doctors began honoring that request—but always with an eye toward safety. “Morphine can be tricky in a very young child,” says Dr. Kost-Byerly. “And medications have side effects: nausea, vomiting, itching.”
According to Dr. Kost-Byerly, the current goal of pediatric pain management is to determine which children have a genetic make-up that would lead them to be sensitive to certain pain meds. She says, “The question we have to ask is: How can we individualize pain medicine?”
Dr. Kost-Byerly and her Hopkins colleagues are working to find that answer. They’re developing the treatments and the equipment appropriate for the tiniest humans—even preemies. “Hopkins is interested in developing a standard of care that can be applied to all children at hospitals across the country,” she says.
Did You Know?
• Sickle cell disease affects different people indifferent ways but almost always includes intense pain. Pain is the most common complication of sickle cell disease and the top reason that people with the disease go to the emergency room or hospital.
• People are born with sickle cell disease; it does not develop in adulthood, and it is not contagious.
• Sickle cell disease is one of the most common genetic diseases in the United States, affecting about 90,000 to 100,000 Americans.
• Sickle cell disease can also cause lung tissue damage and stroke. The blockage of blood flow caused by sickled cells also causes damage to most organs, including the spleen, kidneys and liver.
• Sickle cell disease affects millions of people throughout the world and is particularly common among people whose ancestors come from sub-Saharan Africa, Spanish-speaking regions in the Western Hemisphere (South America, Cuba and Central America), Saudi Arabia, India and Mediterranean countries such as Turkey, Greece and Italy. Because of this, hospitals in the United States screen all newborn babies for sickle cell disease.
PainPathways Magazine
PainPathways is the first, only and ultimate pain magazine. First published in spring 2008, PainPathways is the culmination of the vision of Richard L. Rauck, MD, to provide a shared resource for people living with and caring for others in pain. This quarterly resource not only provides in-depth information on current treatments, therapies and research studies but also connects people who live with pain, both personally and professionally.
View All By PainPathways